What are Neural Implants?
The idea of directly linking the human brain to computers is no longer just science fiction. In the past few years, the idea has moved from theory into real laboratories and even hospital rooms. Neural implants are being developed to reclaim lost abilities, treat neurological disorders, and even augment human functions. Advances in materials science, electronics, and surgery now are enabling the creation of safer, more precise, and more adaptable brain–machine interfaces (BMIs) than ever before. By means of advances in materials science, electronics, and surgery, these devices are emerging from laboratory experiments and moving into clinical practice.
Millions already benefit from neurotechnology, such as cochlear implants for hearing or deep brain stimulation (DBS) for movement disorders. Brain-machine interfaces (BMIs) take this a step further: they record brain activity patterns, decode them, and use the information to power external devices or target therapy. The first implantable BMI in a human was tried out in 2004. Using an array of microscopic electrodes, a paralyzed patient was able to get a computer cursor to move using thoughts alone. Since then, BMIs have progressed to translate imagined handwriting into text, brain activity into speech, and even control robotic limbs. These achievements are proof that implants can decipher subtle, fine-grained signals from the brain.

How Do They Work?
Your brain is speaking in electrical impulses, rapid-voltage shifts between neurons. These signals are quantifiable at multiple levels:
Local field potentials (LFPs): the summation of the activity from many neurons in a small region.
Action potentials ("spikes"): the short firing of a single neuron.
The closer an electrode is to a neuron, the better the signal. That's why implantable devices work so well: they short-circuit the skull and other impediments that degrade and distort signals in non-invasive methods like EEG (Rapeaux & Constandinou, 2021).
Principal types of implantable recording devices:
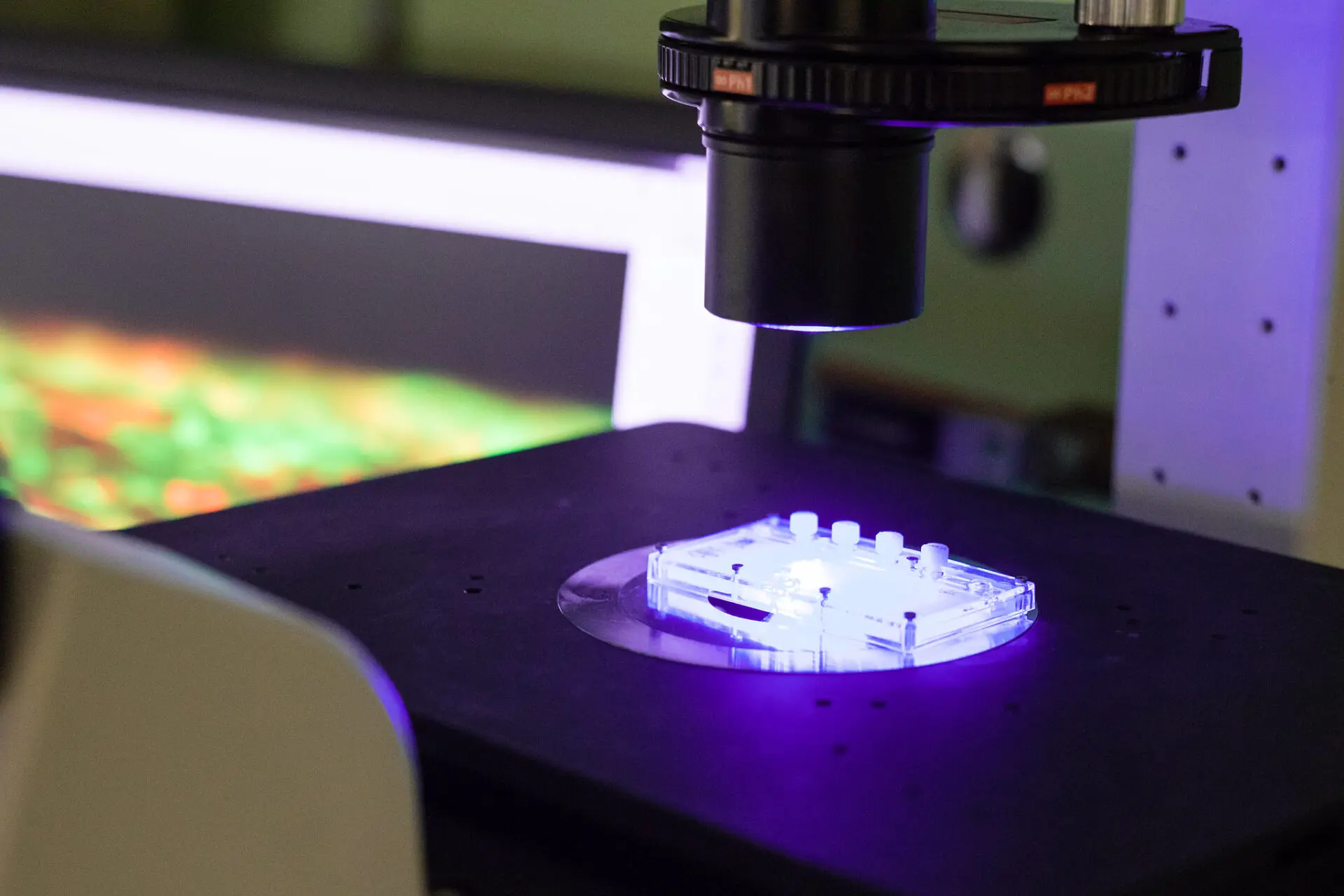
Electrocorticography (ECoG): Thin strips or electrodes implanted on the brain surface. They yield good spatial resolution LFP recording, but will very seldom record individual neurons.
Intracortical microelectrode arrays (MEAs): Tiny needles inserted directly into brain tissue. These can be used to record the firing pattern of single neurons and enable very precise decoding.
Intravascular meshes/stentrodes: Flexible electrode arrays implanted through blood vessels. They can access neurons without the skull needing to be broken, and newer models even observe single-neuron activity (Timko, 2023).
Once implanted, these electrodes measure voltage alterations, which are processed and amplified by onboard or external electronics into digital data. For the implant to be useful, the captured signals need to be transmitted out of the body for processing. This is easier said than done. Wired systems utilize thin wires that travel under the skin, simple but susceptible to infection. Wireless systems utilize radio-frequency (RF) or ultrasonic connections (Rapeaux & Constandinou, 2021; Timko, 2023). Power is conducted into the implant in a similar way, since onboard batteries are usually too big or of too limited a lifespan for continuous use. The two main engineering limitations here are power and heat: implants must operate on an extremely low power budget so that they don't heat brain tissue above 0.5°C. That means data is often compressed or partially analyzed in the implant before it sends it out.
Outside the body, the neural data must be interpreted, which is known as decoding.
It is the process of:
Removing noise and separating spikes from background activity.
Feature extraction: mapping difficult waveforms into simpler, more meaningful measures (e.g., firing rate or signal power in a particular frequency band).
Classification and translation: mapping those features onto a wanted action (e.g., moving a cursor, creating speech sounds, or selecting letters).
More recent BMIs more heavily use machine learning to help decode, account for changing neural signals over time. This is important because electrodes can shift, scar tissue can form, and the brain itself changes with learning and fatigue (Rapeaux & Constandinou, 2021).
Some implants listen but also stimulate the brain. Electrical pulses, light (optogenetics), or even localized heating can be used to activate neural activity.
Examples are:
Restoring motor or sensory function through activation of motor or sensory areas.
Treating epilepsy by detecting the onset of seizures and applying counter-stimulation.
Delivering drugs directly into the brain using biodegradable micro-pumps or heat-assisted diffusion patches (Lee et al., 2021).
Optical stimulation using biodegradable light-guiding fibers that degrade over time.
In two-way BMIs, sensing and stimulation are combined to create closed-loop systems that respond immediately to brain activity.
Flexible and Biodegradable Electronics
Brain tissue is elastic, soft, and fragile. Implants made of hard metals and silicon have traditionally resulted in irritation, inflammation, or scarring in the long term. That's why there's a tremendous shift towards flexible, biocompatible, and even biodegradable materials (Lee et al., 2021):
Flexible polymers (like parylene, polyimide, and PLGA) allow implants to bend with brain tissue.
Biodegradable electronics (e.g., magnesium or molybdenum) and semiconductors (e.g., silicon nanomembranes) degrade harmlessly after they've served their purpose.
Conducting polymers like PEDOT: PSS can provide reasonable electrical performance with a less rigid texture than metals.
Controlling how fast these devices degrade is one of the greatest challenges — too fast, and the device shorts out prematurely; too slow, and it poses an immune risk over the long term.
Traditional neural implants are rigid and permanent. While robust, they are irritating to the brain and typically require surgery for retrieval. Therefore, researchers are crafting flexible, biodegradable devices that bend over the soft tissue of the brain and break down harmlessly when no longer needed.
The machines can monitor brain waves, release medication, or provide electrical or optical stimulation, then break down naturally in days or months. Examples:
Pressure sensors to track swelling after injury.
Photodetectors for the monitoring of surgery optically.
pH and temperature sensors to detect tumors or strokes early.
Drug patches to deliver chemotherapy directly into the brain tissue, by using mild heat to maximize absorption.
Wireless stimulators for ailments like epilepsy or Parkinson's disease.
The primary challenge is controlling how quickly these devices degrade without creating toxic waste products. Some materials being tested include magnesium, silicon nanomembranes, and biodegradable polymers to achieve the optimal balance of performance and safety.
More Data, More Challenges
Present-day BMIs aim to record hundreds or thousands of channels in real time. The more electrodes, the more data, which potentially facilitates smoother control of prosthetics or faster decoding of speech. But it also presents technical hurdles: implants need to transmit enormous amounts of data without getting hot, be small enough to fit inside the skull, and work properly for decades.
One of the most promising ideas is called the distributed approach, scattering many tiny, wireless implants (neurograins" or "neural dust") across different areas of the brain. This would be less invasive with broader coverage. But more information isn't always better: neural signals change over time, requiring repeated recalibration, and decoding software must function within the tight power budgets of an implant.

From Labs to Clinics
Neural implant technology is attracting significant commercial investment. Blackrock Neurotech, Synchron, Paradromics, and Neuralink are developing various approaches, from high-density electrode arrays to stentrodes and flexible threads. The goal: make implants safer, more durable, and convenient enough for everyday clinical use. There are still obstacles, such as proving long-term safety and obtaining regulatory approval, before these technologies reach the mainstream.
Conclusion
Imagine a machine that senses the beginning of a seizure and gives medicine to the affected area before a person even feels any symptoms or a system that brings a person back from a stroke with normal speech by translating words in real time. With elastic materials, minimally invasive delivery of drugs, and smarter decoding algorithms, those scenarios could become a reality.
Neural implants sit at the intersection of biology, engineering, and medicine. If we maintain the pace we are now going, we are soon going to be into a time when mind and machine become best of friends, not science fiction, but everyday healthcare.
References
Lee, W. H., Cha, G. D., & Kim, D.-H. (2021). Flexible and biodegradable electronic implants for diagnosis and treatment of brain diseases. Current Opinion in Biotechnology, 72, 13–21. https://doi.org/10.1016/j.copbio.2021.07.027
Rapeaux, A. B., & Constandinou, T. G. (2021). Implantable brain machine interfaces: First-in-human studies, technology challenges and trends. Current Opinion in Biotechnology, 72, 102–111. https://doi.org/10.1016/j.copbio.2021.10.001
Timko, B. P. (2023). Neural implants without brain surgery: Injectable bioprobes record single-neuron activity from within blood vessels. Science, 381(6655), 268–269. https://doi.org/10.1126/science.adi9330